Experts estimate that there are more than 10,000 prescription medications available in the United States alone, in addition to compound medications and biological products. Given the high number of medications handled and dispensed by pharmacies, many of which can cause health problems when inhaled, maintaining proper air quality is essential to safeguarding pharmacy professionals and equipment by reducing exposure to harmful airborne contaminants.
Of course, many people with a wide range of communicable diseases visit pharmacies throughout the day. From the common cold and influenza to COVID-19, airborne diseases caused by viruses and bacteria are common in pharmacies. Modern air filters and properly designed air filtration and ventilation systems play a vital role in preventing the spread of disease in these environments.
The Crucial Need for Air Quality in Pharmacies
Protecting the health of pharmacists, staff, and customers is clearly the top priority when developing a strategy for maintaining clean air in a pharmacy setting. Pharmacies are considered high-risk areas for exposure to airborne contaminants, including those emanating from medications, as well as allergens, particulate matter, volatile organic compounds (VOCs), viruses, and bacteria. Contamination can even trigger allergic reactions.
Air quality is also critical in ensuring the purity and efficacy of drugs that are processed in pharmacies. Medication can become unsafe or ineffective when contaminated with airborne pollutants. This is especially true of sterile medication, which must not be exposed to contaminants in order to minimize the risk of infection. High temperatures and humidity levels can cause medication to degrade over time. Poor air quality exacerbates this degradation, making medication less effective or potentially unsafe while reducing its shelf life.
Because of the role pharmacies play in healthcare, regulatory and compliance standards must be met to keep patients safe and ensure medication is effective. These include:
- Federal standards
- Controlled Substances Act (CSA)
- Food, Drug, and Cosmetic Act (FD & C Act)
- Prescription Drug Marketing Act (PDMA)
- Medicare and Medicaid regulations
- State regulations involving pharmacy licensing, prescription requirements, and reporting
- Additional standards
- Joint Commission (JC) for pharmacies affiliated with hospitals and healthcare facilities
- American Society of Health-System Pharmacists (ASHP) guidelines and best practices
- National Council for Prescription Drug Programs (NCPDP) standards for electronic prescriptions and technology
The National Alliance of State Pharmacy Associations (NASPA) and the American Pharmacists Association (APhA) offer resources to help pharmacies comply with various regulations, including those related to air quality, to ensure a safe environment.
Potential Airborne Contaminants in a Pharmacy Environment
Airborne contaminants from drugs, solvents, and chemicals can create a variety of health risks, including respiratory problems, reproductive issues, skin irritation, and even cancer. For example:
- Prolonged exposure to antibiotics can contribute to resistance to those antibiotics in bacteria.
- Common solvents such as benzene have been linked to cancer and can cause skin irritation, neurological issues, and other health problems.
- Chemicals in widely used cleaning products can be harmful if inhaled and irritate the eyes, nose, and throat.
Airborne pathogens such as viruses, bacteria, and fungi are a serious threat to drug safety. Drugs can become contaminated during storage or dispensing, while cross-contamination between different medication can occur through the air. Both contribute to reduced effectiveness, degradation, infection, and adverse reactions in patients.
Chemical fumes can also contaminate medication and create health risks similar to those mentioned previously. For example:
- Cytotoxic drugs can be toxic, damage healthy cells and tissues, and increase the risk of cancer and reproductive issues.
- Antineoplastic drugs can be toxic, damage bone marrow, and increase the risk of anemia and neutropenia.
Air Filters: Designed for Pharmacies
Air filters protect people, medication, and equipment by removing a wide range of airborne particles, including dust, pollen, mold spores, bacteria, and viruses, as well as chemicals, gases, and odors. Air filters trap particles to remove them from the air and prevent them from being circulated through the pharmacy space. Filters also help to maintain consistent temperatures and humidity levels.
Several different types of air filters are used in pharmacies:
- General ventilation air filters are commonly tested and classified according to the MERV scale as defined in ASHRAE Standard 52.2. The range of MERV-rated filters runs from 1-16 and can have an average efficiency as high as 95% on particles between 0.3 microns to 1.0 microns. The filters are used as the primary air filter for incoming air through HVAC systems and as prefilters to HEPA and ULPA filters.
- High-efficiency particulate air (HEPA) filters that are tested and certified can capture a minimum of 99.97 percent of airborne particles that are 0.3 microns or larger, including bacteria and viruses. These filters are essential in pharmacies that handle sterile medications, cytotoxic drugs, and other medications that are sensitive to contamination.
- Ultra-low penetration air (ULPA) filters are even more efficient than HEPA filters and are designed to capture a minimum of 99.9995 percent of airborne particles that are 0.12 microns or larger. They are ideal for cleanrooms, sterile compounding labs, and other spaces that require exceptionally clean air
- Molecular air filters have a large surface area of activated carbon that adsorbs molecules to remove volatile organic compounds, strong odors, and hazardous gases. Activated carbon filters are often used in tandem with general ventilation filters and sometimes even HEPA filters as part of a comprehensive air filtration system.
The minimum efficiency reporting value (MERV) rating system uses a scale of 1 to 16 to indicate a filter’s effectiveness in removing particles. The higher the rating, the higher the efficiency, and the smaller contaminant the filter is capable of capturing. General ventilation air filters with a minimum rating of MERV 13 or higher are typically recommended for pharmacies, while HEPA or even ULPA air filters are generally used for cleanrooms, compounding labs, and other areas that require exceptional air quality.
Challenges in Maintaining Pristine Air Quality in Pharmacies
Any discussion about obstacles to clean air in pharmacies must begin with medications, many of which have chemicals or VOCs that can be dangerous if inhaled. Given the hundreds or even thousands of drugs handled in a pharmacy, plus compounds, simply identifying the potential risks can be challenging.
Pharmacy design has a direct impact on air quality. Tight spaces, high foot traffic, porous materials like carpet and fabric upholstery, poorly designed airflows, and insufficient ventilation, can contribute to higher levels of pollutants in the air and on surfaces. Open storage of medication and hazardous materials can allow harmful fumes and VOCs to be released into the air.
When designing a pharmacy, separate areas for medication and hazardous materials, cleaning supplies, waste disposal, and customer interactions are recommended. Smooth surfaces, airtight storage, natural light, proper ventilation, and negative pressure isolation in compounding areas, high-tech machine zones, and other sensitive areas will help overcome these challenges, resulting in cleaner air.
Choosing the Right Air Filter for Pharmacies
There are many factors that must be taken into consideration when choosing air filters for a pharmacy.
- Pharmacy size. High-efficiency filters with lower resistance to airflow are preferred for larger pharmacies to support a higher volume of circulating air.
- Range of drugs processed. As discussed previously, different types of medication create a variety of risks, each of which must be addressed.
- Types of machinery. The operation of highly sensitive equipment can be negatively affected by poor air quality.
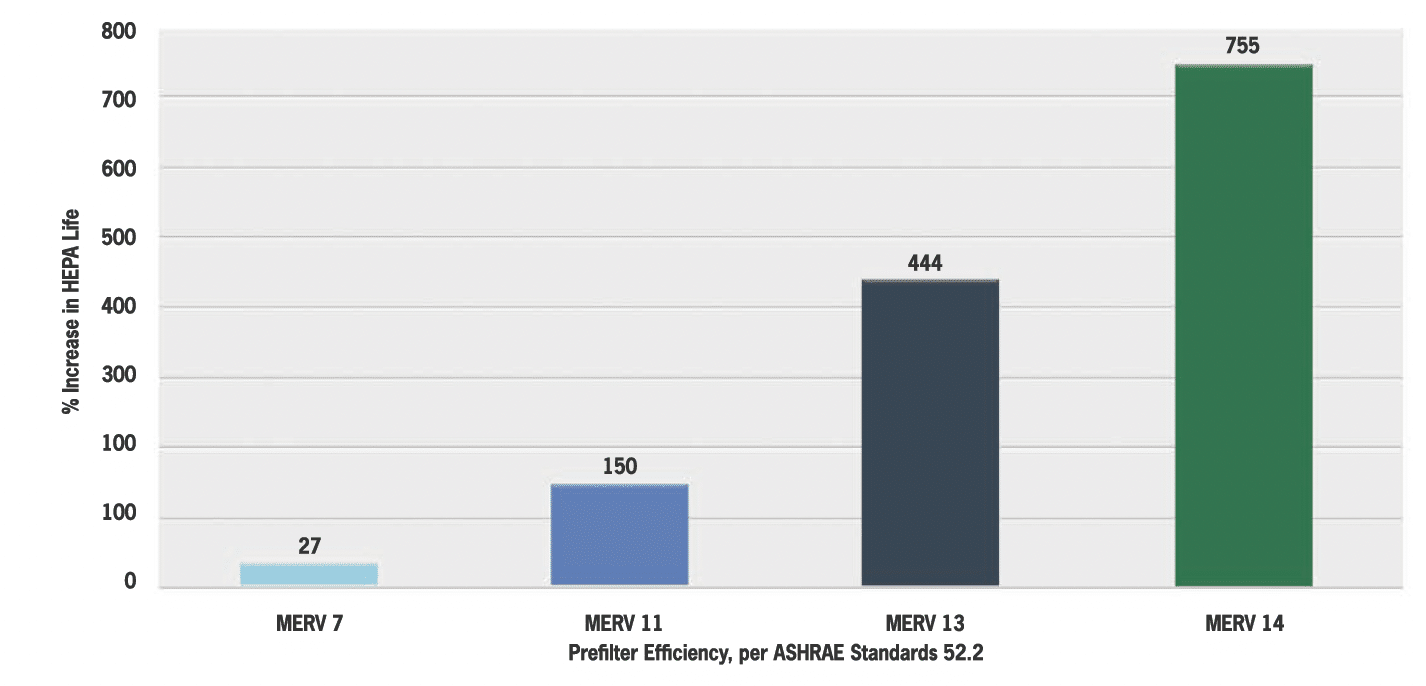
Organizations also must strike the right balance between cost, efficiency, and maintenance needs. High-efficiency air filters are more expensive and typically require one or more stages of prefiltration installed in front of them which must be changed out more frequently. Proper prefiltration will help increase the longevity and efficiency of the expensive final filters. Following good maintenance practices for both air filters and the entire HVAC system will help you maintain clean, safe air with greater consistency. At the same time, regulations and compliance standards for safety and air quality must be met, regardless of cost and maintenance.
Implementation and Maintenance: A Pharmacy Focus
Best practices for installing air filters in critical pharmacy areas should be followed to protect staff, customers, medication, and machinery. In addition to choosing the right filter based on the activities, materials, and occupants in each space, the filter must be compatible with the air handling unit, which should be cleaned prior to installation. Installers should follow best practices and regulations in their area such as wearing rPPE for their own safety and avoid touching the media filter to prevent contamination.
Filter type and date of installation should be documented and referenced for scheduling maintenance and filter replacement. Generally, filters should be replaced when accumulating dirt has restricted airflow through the filter to a predetermined point which could be different based upon the specific application.
However, air filters and the air handling unit should be inspected regularly to determine if the maintenance plan should be updated.
While the right equipment is essential, staff must be trained to recognize the importance of air quality and relevant regulations. They should learn how air filtration works, how to identify warning signs that air filters are not functioning properly, and what steps to take if problems are suspected.
Conclusion: Elevating Pharmacy Standards with Clean Air
Air quality is absolutely essential to creating and maintaining a safe pharmacy environment for pharmacists, staff, and customers. A high-quality air filtration system will dramatically reduce the risk of contamination of medication and equipment, prevent the spread of airborne pollutants, and ensure compliance with federal, state, and industry regulations.
With compliance requirements likely to increase in number and complexity and heightened awareness of the risks involved with airborne pollutants, the contribution of air filters to modern pharmacy operations is undeniable. Manufacturers must continue to innovate, and pharmacies must invest in modern air filters and expertly designed air filtration systems to optimize air quality and cost-efficiency.
If you would like to discuss your pharmacy’s air filtration needs and challenges and learn more about Camfil solutions, please contact us today for a consultation.
The post Commercial and Public Building Air Filters for Pharmacies: Ensuring Safe and Efficient Operations appeared first on Air Filters for Clean Air.
from Air Filters for Clean Air
 It’s important to note that HEPA filters typically don’t function independently in an operating room’s ventilation system. A comprehensive overview below explains how various filters can collaborate or tackle specific challenges in surgical environments.
It’s important to note that HEPA filters typically don’t function independently in an operating room’s ventilation system. A comprehensive overview below explains how various filters can collaborate or tackle specific challenges in surgical environments.
 Molecular Air Filters
Molecular Air Filters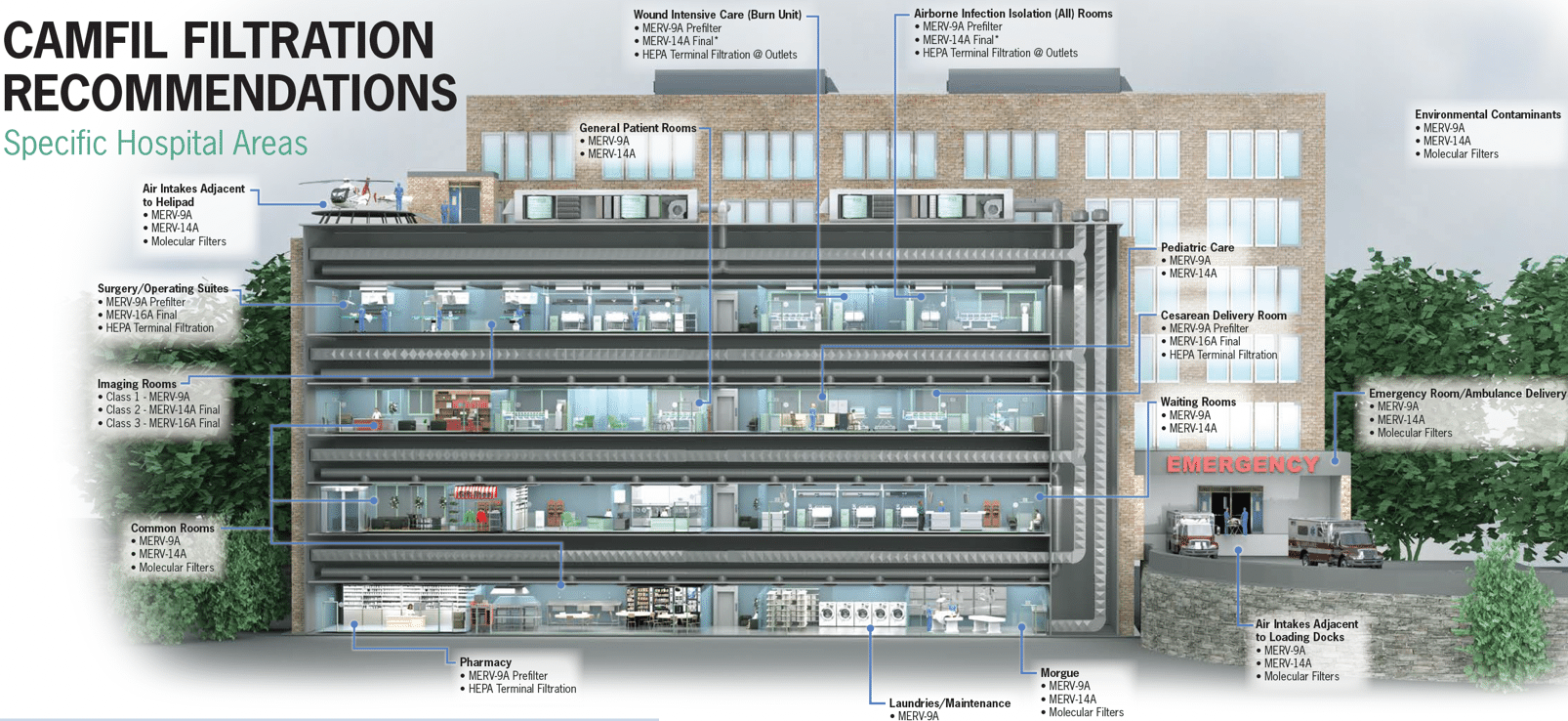 By choosing the right filter or combination of filters, healthcare facilities can greatly improve indoor air quality. This not only aids in infection control but also fosters a safer and more conducive environment for patient recovery.
By choosing the right filter or combination of filters, healthcare facilities can greatly improve indoor air quality. This not only aids in infection control but also fosters a safer and more conducive environment for patient recovery.